‘Is it hot flashes or hot flushes?’(*Find out at the end of the article)
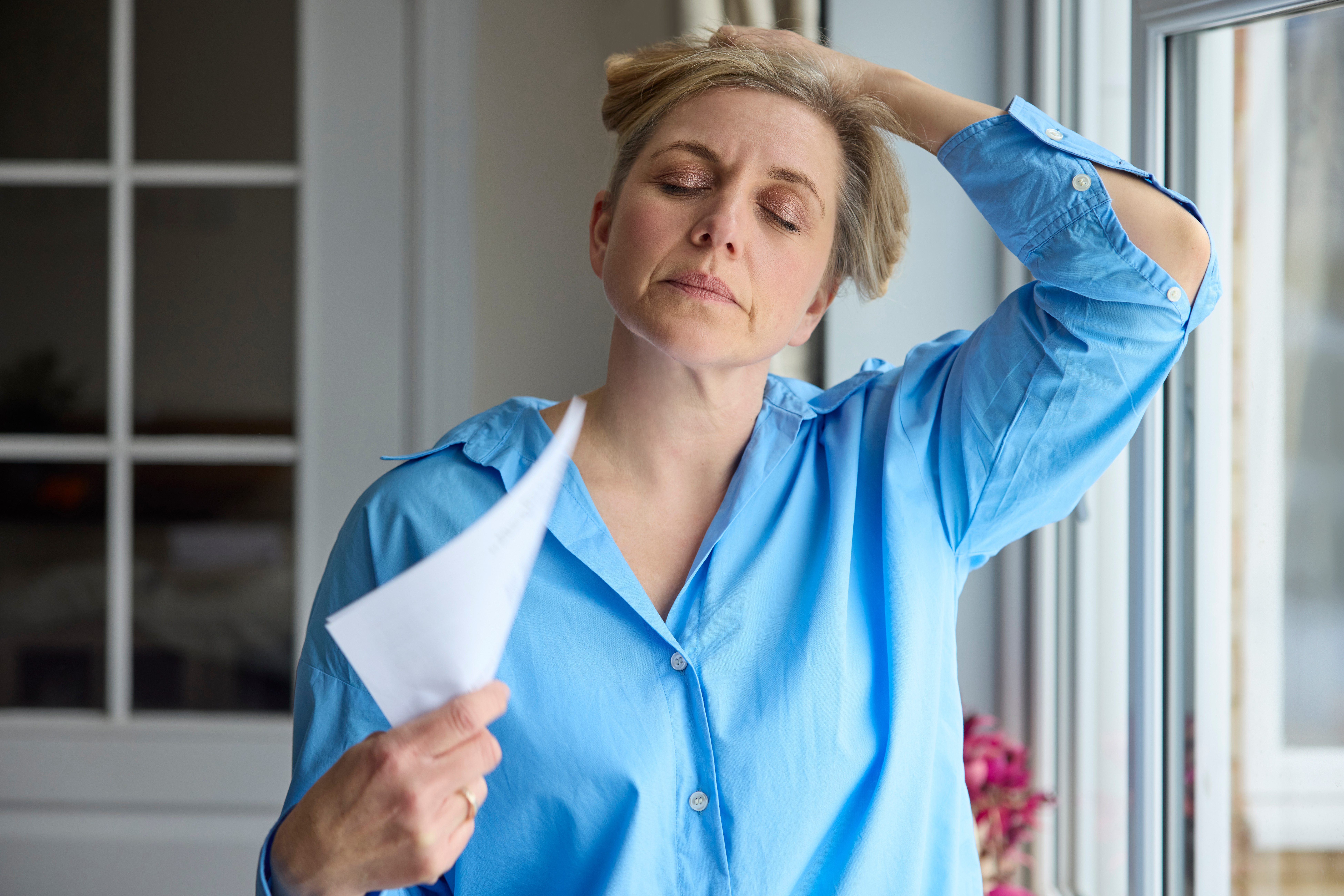
Whatever you choose to call them, hot flushes are an often uncomfortable and unpredictable symptom of menopause. They’re also one of the most common perimenopause and menopause symptoms, with 8 out of 10 menopausal women experiencing them.
So, take a nice, deep breath as we take a deep dive into the causes and triggers of hot flushes. You’ll also discover some helpful hot flush management strategies to add to your menopause management toolkit.
What Are Hot Flushes?
Imagine the top half of your body is suddenly teleported into an overly hot sauna. Your skin reddens, you feel warm, and you start to sweat. Hot flushes can feel a bit like that.
Hot flushes may:
- Feel like warmth starting in your chest and spreading over your neck and face.
- Involve reddening and blotchiness of the skin.
- Occur with a rapid heartbeat.
- Cause mild or profuse sweating. Profuse sweating that happens at night is called night sweats.
- Leave you feeling chilled after it passes.
The intensity of hot flush symptoms is a spectrum. They can be mild and not bothersome, uncomfortable and possibly distressing (especially if you’re in a work or social setting) or somewhere in between.
They don’t usually happen in a predictable pattern. Hot flush experiences vary widely in women going through the menopausal transition. Some women never have them!
A hot flush may be quick (a few seconds) and occasional, though some people have more than 20 hot flushes a day.
Most women will experience hot flushes during perimenopause and menopause. They may happen, at varying frequencies, for around 5 years. However, some women experience them for more than 10 years.
What Causes Hot Flushes During Menopause?

The cause of hot flushes has not been well understood and is still being studied. Research suggests that hot flushes during menopause happen because levels of the hormone Oestrogen drop. This change affects a part of the brain that controls body temperature, making it more sensitive than usual. As a result, even small changes in body heat can trigger sudden feelings of warmth, sweating, and flushing – what we know as a hot flush.
Some triggers of hot flushes:
- caffeine
- alcohol
- hot drinks
- spicy foods
- stress
- anxiety
Natural and Lifestyle-Based Strategies for Managing Hot Flushes
The three main lifestyle strategies for managing hot flushes involve diet, exercise and stress management.
Dietary changes to manage hot flushes

The main dietary change you need to make to avoid hot flushes is to work out what foods or beverages trigger them. Try keeping a food diary for a few days or weeks and noting when you have a hot flush.
Some of the usual suspects that trigger hot flushes are caffeine, alcohol, hot drinks and spicy foods.
Exercise and hot flushes

We all know that regular physical exercise has a wealth of mind and body benefits. But, the scientific evidence is less clear about the specific effects of exercise on hot flushes.
The main problem is that exercise for hot flush improvement has not been well studied in the past. Older research suggests that regular exercise has a limited effect on hot flushes. A more recent study, on the other hand, reveals that many women felt that exercising helped their hot flushes and night sweats.
We do know that regular exercise helps many of us manage stress and anxiety, which are well-known triggers of hot flushes.
We also know that exercise, along with a calorie-restrictive diet, helps with weight loss. Losing weight could help ease your hot flushes.
Stress management strategies for hot flushes

Managing your stress can impact your hot flushes, especially with how much your symptoms worry you.
- Cognitive behavioural therapy (CBT). Evidence suggests that this type of counselling helps to ease how much hot flushes bother you.
- Mindfulness meditation. This is a type of breathing and relaxation meditation might ease mild hot flushes.
- Hypnosis. There is research showing that hypnosis might help both how often you get hot flushes and how bad they are.
It’s best to seek help from an accredited clinical professional for any of these strategies.
When to Consider Hot Flush Treatment Options
If your hot flush symptoms start to affect your quality of life or your sleep, there are treatments that can help. Options include over-the-counter products and medicines requiring a doctor’s prescription.
Hot-flush treatments available over-the-counter from your pharmacy include products that contain:
- Black Cohosh
- Plant estrogens
- Vitamin E
Remifemin, with the natural active ingredient, Black Cohosh, supports menopause symptom relief by reducing hot flushes and night sweats

It’s always best to discuss your symptoms and concerns with your doctor, as they are best placed to offer treatment guidance that’s right for you.
A number of different prescription medicines options can be used to manage menopausal symptoms. But before prescribing, ask your doctor to check your medical history and consult your treatment preferences. It’s important that you fully understand the pros and cons of your treatment options. Some medicines are not suitable for some women.
*Do you say hot flushes or hot flashes? Hot flushes is the term generally used here in Australia, while hot flashes is the term preferred in the USA.